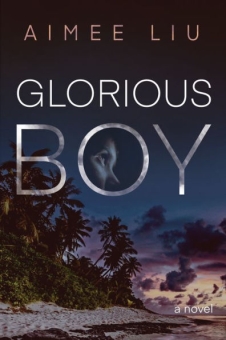
Le Garcon Magnifique
Glorious Boy in French translation,
published by Mercure de France!
Glorious Boy is also available as an audiobook!
"The most memorable and original novel I've read in ages… evokes every side in a multi-cultural conversation with sympathy and rare understanding."
– Pico Iyer, author of Autumn Light
Finalist for the 2020 Staunch Book Prize
BOOKLIST'S TOP 10 HISTORICAL FICTION OF 2020
Good Housekeeping's "Best Books of 2020"
Brit+Co's 12 Books That Will Take You on a Literary Vacation
A tale of war and devotion, longing and loss, and the power of love to prevail…
“Reminiscent of the tone and atmosphere of Somerset Maugham and George Orwell’s Asia-set novels, Glorious Boy is a Second World War story of adventure and loss, uniquely set in the Andaman Islands, one of India’s farthest flung territories” – Asian Review of Books
"In 1942, Claire Durant waits with her husband and young son for the all-clear to leave the Andaman Islands, where they’ve been stationed since 1936. The Andamans, east of India in the Bay of Bengal, are home to a colony of Burmese and Indian convicts as well as the native people, the Biya. Claire, a budding anthropologist, has been studying the Biya and getting to know them, but as WWII intensifies, she has no choice but to leave the people she loves. There is one other complication: Naila, their young servant, has a special relationship with Claire’s son, Ty. And when Naila disappears with Ty, there’s no telling what will happen to the family as they are wrenched apart. This fascinating novel examines the many dimensions of war, from the tragedy of loss to the unexpected relationships formed during conflict. The Andamans are a lush and unusual setting, a sacred home to all kinds of cultures and people, and Liu’s prose is masterful. A good choice for book groups and for readers who are unafraid to be swept away." --Booklist STARRED review
Subscribe to Aimee's newsletter HERE
To read an Excerpt from Glorious Boy
OF THE ANDAMAN ISLANDS
Read Aimee's essay on the origins of Glorious Boy in LitHub --HERE
Latest Blog posts:
New Resource Newsletter for Creative Writers
_w140_h140/MFA%20Lore%20Logo(1)_06250834.png)
I’ve just launched a new section at my Substack publication, Legacy & Lore especially for writers of creative nonfiction and fiction. MFA Lore is meant to share the wealth that I’ve gleaned over more than four decades of publishing and teaching creative writing at the MFA level.
Why MFA Lore? I know there’s some dispute about the value of graduate degrees for writers who “just want to write.” I shared that hesitation for years, publishing more than three novels and four nonfiction books before getting my own MFA at Bennington. But the knowledge, insight, and community I gained at Bennington ignited my writing life and improved my work in too many ways to count. My goal here is not to motivate you to get an MFA (unless you’re so inclined, of course) but to give you a taste of the wisdom I’ve absorbed while studying and teaching in an MFA program.
You can check it out and subscribe HERE
The 3 M's That Forecast a Bestseller
_w140_h140/Image%20-%20no%20preview%20-%20square(2)_01250724.jpg)
Hi Everyone,
This past week I had the privilege of chatting with several senior editors and publishers from major houses in NY. All were interested in the new book I’m ghosting and, while I can’t tell you anything about our specific project, I did pick up an editorial formula that might interest you. It’s how one publisher predicts which books will be bestsellers.
Subscribe and read the full article HERE!
Power Up Your Passive Protagonists!
Hello everybody,
Here's the latest from my MFA Lore newsletter on Substack
I’m back in the MFA archives again, mining gems that could bring value to your writing life. Today’s diamond in the rough is a letter about passive protagonists that I wrote to one of my most talented MFA advisees. With her permission, I’m going to share pertinent sections of this letter with you because, over the years, I’ve found that many, if not most of us, unwittingly hobble our protagonists in the inception. Activating them, then, becomes a priority in revision.
This advice is geared primarily toward fiction writers, but I urge memoirists to take note, too. When we write our own stories, we need to cast ourselves as active narrators, plunging into the past to rescue buried truths. There’s nothing passive about that role, yet it can be difficult to see and write ourselves onto the page in a truly active voice.
Passive protagonists and narrators are especially common in the work of female writers born into generations that discouraged or prevented women from speaking up, acting on their desires, and fighting for their rights. Women who were raised to hold themselves back, to mind their tongue, suppress their desires, and behave like “ladies,” could be forgiven if they struggled to speak their minds and demand the attention they deserved. For more than a century, then, the muted struggle between expression and restraint supplied the dramatic tension at the heart of fiction like Kate Chopin’s The Awakening, Sylvia Plath’s The Belljar, and Virginia Woolf’s To The Lighthouse. But interest in such straitjacketed characters has waned in the era of Olive Kitteridge, Lisbeth Salander, and Hermione Granger. And that’s a problem for writers like me.
Visit MFA Lore @Substack to read the whole articleIntricacies of POV
This is the biweekly writers’ Q&A from the MFA Lore section of Aimee Liu's Legacy & Lore newsletter @Substack.
Become a paid subscriber HERE to read the whole Roundup.
Welcome to our second Roundup, everyone!
I appreciate this week’s terrific questions. I’m in the thick of these same issues with my own work, so it was good to give them a bigger think here.
Before we plunge in, please remember that writing is a game that requires us to break as many rules as we observe. Prescriptions are for pharmaceuticals, not literature. So, while these answers reflect my literary preferences and experience as an author and teacher, they’re only my advice. Never forget that you are the author of your work, so the ultimate decision for what goes on in your pages lies with you.
A book promotion 101 lesson from Oprah herself
You know what they say about best laid plans? Well, that goes double when Oprah calls. Even when she doesn’t call you.
Last week I was thrilled to be asked to “chat” onstage with novelist and physician extraordinaire Abraham Verghese for the series Live Talks Los Angeles. Though I’d never before met him, I’d loved Verghese’s first novel, Cutting For Stone, when it came out a decade ago. I’d traveled in Kerala, India, the location of his new novel, The Covenant of Water, and I’d written two novels of my own about India during the same turbulent colonial period when most of this story takes place. So I knew we’d find a lot to talk about.
I’ve interviewed others for Live Talks, including Aimee Tan and Pico Iyer. I prepare diligently for these events, both as a sign of respect for the authors and also as the best strategy for managing my own stage fright before large audiences. For this conversation I needed to inhale all 724 pages of The Covenant of Water inside of a week. I had to get cozy with more than 30 key characters and their masterfully interwoven plot lines. I needed to absorb the whole multi-generational saga so I could discuss its vast scope and humanity in detail. Or so I thought.
What I didn’t know was that The Covenant of Water would be selected for Oprah’s book club the week of our chat. And what I didn’t factor into my preparation was the fact that we’d be discussing the novel just one day after its publication date.